What are Spine Deformities?
Spine deformities refer to abnormal curvatures or misalignments of the spinal column, which disrupts its natural structure and functionality. A healthy spine features a natural curvature that helps in bearing weight and maintaining balance. However, in the case of spinal deformities, such as scoliosis, lordosis, and kyphosis, these curves may become exaggerated or diminished, leading to potential complications in movement and overall health.
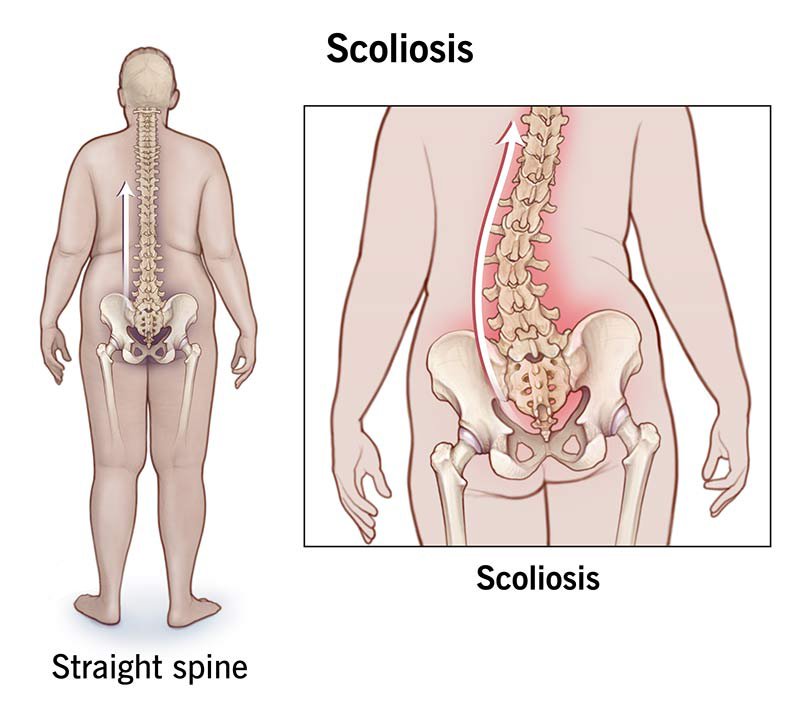
Scoliosis is characterized by an abnormal lateral curvature of the spine, often shaped like an “S” or “C.” This condition can develop during adolescence but can also arise in later stages of life. Lordosis involves an exaggerated inward curvature of the lower back, which can cause discomfort and pain. Conversely, kyphosis presents as an excessive outward curvature of the upper back, commonly referred to as hunchback. Each of these deformities significantly alters the alignment of the spine and can affect bodily functions, including respiration and posture.
The anatomy of the spine is made up of various components, including vertebrae, intervertebral discs, nerves, and muscles, all of which work cohesively to support the body. Deformities can arise from numerous factors, including genetic predispositions, where inherited conditions manifest into spinal irregularities. Neuromuscular diseases can also lead to abnormalities in the spine as they weaken the muscles and disrupt the ability to maintain proper posture. Additionally, developmental issues during childhood may contribute to the formation of these conditions. Understanding the mechanics and causes of spine deformities is crucial in formulating effective treatment and management strategies.
Understanding Scoliosis: Causes and Symptoms
Scoliosis is a complex spinal deformity characterized by an abnormal lateral curvature of the spine, which can manifest in several forms. The most prevalent type is idiopathic scoliosis, often developing during adolescence without a known cause. This form typically arises just before puberty, leading to noticeable curvature that can worsen as the individual grows. It is crucial to monitor children and adolescents for potential signs, especially as they approach these growth spurts.
Congenital scoliosis stems from spinal deformities present at birth, caused by malformations in the vertebrae. These abnormalities can lead to significant curvature as the child ages, emphasizing the need for early detection. Neuromuscular scoliosis, on the other hand, is associated with neuromuscular conditions such as cerebral palsy or muscular dystrophy. In these cases, the muscles that support the spine are unable to function optimally, leading to curvature due to weakness or imbalances.
Common symptoms associated with scoliosis include uneven shoulders, which may appear due to one shoulder being higher than the other, and a prominence of one hip aligning differently from its counterpart. An asymmetric waist is another hallmark sign, where one side may appear more protruded or elongated than the other. These physical manifestations can affect a person’s posture and overall appearance, leading to potential self-esteem issues.
Recognizing these symptoms early is paramount. Parents and caregivers should seek medical advice if they observe any signs of scoliosis in a child, particularly during growth periods. Early diagnosis can be instrumental in managing scoliosis effectively, as treatment options may become more limited with increased severity. Timely intervention can greatly reduce complications and improve quality of life for individuals affected by this condition.
Diagnosis and Treatment Options for Scoliosis
Diagnosing scoliosis typically begins with a thorough physical examination conducted by healthcare professionals. During the examination, the provider often checks for any visible signs of spinal deformities, such as uneven shoulders, hips, or a prominent rib cage. In many cases, forward bending tests are performed to accurately assess spinal curvature, which helps determine the severity of the condition. If scoliosis is suspected, imaging tests are essential for confirmation and further evaluation. Common imaging modalities include X-rays, which provide a clear view of the spine’s alignment and curvature, and MRIs, offering additional details regarding spinal cord integrity and other soft tissue structures.
Upon diagnosis, treatment options for scoliosis vary depending on the severity of the curvature and the age of the patient. For mild cases, healthcare professionals may recommend careful observation and regular follow-up appointments to monitor any changes in spinal curvature. In instances where scoliosis progresses, especially in children, bracing might be advised. Bracing aims to halt the progression of spinal deformity by applying pressure to the spine until the skeleton matures.
In more severe cases, surgical intervention becomes necessary. Surgical options, such as spinal fusion, can correct the curvature and stabilize the spine, ensuring that further complications are prevented. The decision for surgery generally weighs factors like degree of curvature, age of the patient, and overall health. Physical therapy is another integral component of scoliosis management, often used to strengthen spinal muscles and improve flexibility. Additionally, alternative treatments like chiropractic care and yoga may provide symptomatic relief, although scientific support for these methods is variable. A comprehensive treatment strategy tailored to each individual is crucial for effectively managing scoliosis and enhancing overall well-being.
Living with Scoliosis: Coping Strategies and Support
Living with scoliosis can present various challenges, both physically and emotionally. Understanding these challenges is crucial for individuals diagnosed with this spinal condition. Coping strategies that focus on enhancing physical well-being can greatly improve quality of life. Regular exercise tailored to individual capabilities, such as swimming or yoga, can help strengthen core muscles, improve flexibility, and alleviate discomfort associated with scoliosis. Engaging in low-impact aerobic activities can promote cardiovascular health while being mindful of spinal alignment.
In addition to physical exercises, making ergonomic adjustments in daily life is essential. Maintaining proper posture while sitting, standing, and lifting can significantly reduce strain on the spine. Individuals should use supportive chairs and desks when working or studying, ensuring their workstation is well-designed to suit their needs. Simple adjustments, such as using a cushion for lumbar support or adjusting the height of screens, can contribute positively to overall comfort during daily activities.
Emotional and psychological support plays a critical role in coping with scoliosis. Many individuals find solace in connecting with others who share similar experiences. Joining support groups can offer a sense of community, where members can discuss their challenges, share coping strategies, and provide encouragement. Additionally, seeking professional counseling can be beneficial for those struggling with self-image or anxiety related to their condition.
Implementing a holistic approach that includes physical therapies and emotional support can empower individuals living with scoliosis. By embracing coping strategies, fostering connections, and adapting their lifestyle, individuals can lead fulfilling lives despite the challenges posed by this spinal deformity. As they navigate their journey, access to resources and a supportive network is paramount in instilling resilience and encouraging positive adaptation to scoliosis.
Frequently Asked Questions ?
1. What is scoliosis?
Answer: Scoliosis is a condition where the spine curves abnormally to the side, forming an “S” or “C” shape when viewed from behind. This curvature can vary in severity and may cause uneven shoulders, hips, and in some cases, back pain. Scoliosis often develops during adolescence but can occur in people of all ages.
2. What causes scoliosis?
Answer: The exact cause of scoliosis is often unknown (idiopathic scoliosis), especially in adolescents. Other types, like congenital scoliosis, result from vertebral malformations present at birth, while neuromuscular scoliosis is associated with conditions like cerebral palsy or muscular dystrophy. Degenerative scoliosis may develop later in life due to aging.
3. Who is at risk for scoliosis?
Answer: Scoliosis can affect anyone, but it is most commonly diagnosed in children between the ages of 10 and 15, with girls being more likely to experience severe curves. Having a family history of scoliosis also increases the risk, as does having certain neuromuscular conditions.
4. What are the signs and symptoms of scoliosis?
Answer: Symptoms of scoliosis include uneven shoulders, a noticeable curve in the spine, uneven hips, or one side of the ribcage sticking out more than the other. In severe cases, it can lead to back pain, difficulty breathing, or other complications due to pressure on the internal organs.
5. How is scoliosis diagnosed?
Answer: Scoliosis is diagnosed through a physical examination and imaging tests, such as X-rays, to measure the degree of spinal curvature. The doctor may use the Cobb angle to determine the severity of the curve and guide treatment recommendations.
6. What are the treatment options for scoliosis?
Answer: Treatment depends on the curve’s severity, the patient’s age, and whether the curve is progressing. Mild cases may require observation only. Moderate cases might be treated with a brace to prevent further curvature in growing children, while severe cases may need surgical correction, such as spinal fusion.
7. Does scoliosis worsen over time?
Answer: In some cases, scoliosis can worsen, especially during growth spurts in adolescence. Curves in adults may also progress due to aging and degeneration. Regular monitoring and timely intervention can help prevent worsening of the condition.
8. Can scoliosis cause pain or other complications?
Answer: Mild scoliosis usually does not cause pain. However, severe or progressive cases can lead to back pain, reduced mobility, and respiratory issues if the curve compresses the lungs. Degenerative scoliosis in adults may lead to chronic pain and functional limitations.
9. Can scoliosis be prevented?
Answer: There is currently no known way to prevent idiopathic scoliosis, as its cause is largely unknown. However, early detection and treatment can manage the condition effectively and prevent further complications. Exercises and physical therapy may help maintain flexibility and muscle strength.
10. How can scoliosis impact daily life, and how can people manage it?
Answer: The impact of scoliosis on daily life varies. Mild scoliosis may have little to no effect, while severe cases can lead to physical limitations or self-consciousness about appearance. Management strategies include regular exercise, maintaining good posture, and following treatment plans prescribed by healthcare providers. Support groups and education can also help individuals cope emotionally with scoliosis.