What Causes Osteoarthritis?
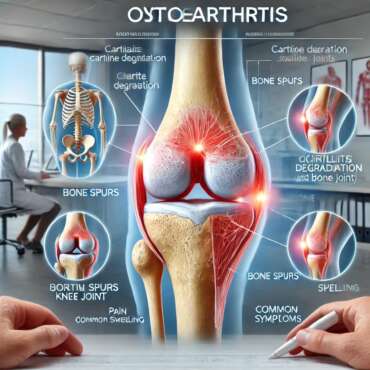
Osteoarthritis is a complex degenerative joint disease characterized by the gradual breakdown of cartilage, which serves as a cushion between bones in a joint. The deterioration of this cartilage results in increased friction and inflammation, leading to pain and stiffness. At a biological level, several mechanisms contribute to the onset and progression of osteoarthritis. Factors such as aging, along with joint wear and tear, significantly influence the development of this condition. As individuals age, cartilage naturally loses its elasticity and resilience, rendering the joints more susceptible to damage.
Beyond the aging process, genetics plays a crucial role in the predisposition to osteoarthritis. Research indicates that individuals with a family history of osteoarthritis are more likely to develop this condition, suggesting a heritable component that may affect cartilage composition and joint structure. Additionally, obesity is a significant risk factor; excess weight increases stress on weight-bearing joints, accelerating the wear and tear of cartilage over time. This correlation between body mass index (BMI) and osteoarthritis prevalence highlights the importance of maintaining healthy body weight as a preventive measure.
Joint injuries, whether from sports, accidents, or other physical activities, can also serve as precursors to osteoarthritis. Injuries may cause lasting damage to the cartilage and surrounding structures, increasing the likelihood of developing osteoarthritis in the affected joints. Furthermore, certain metabolic diseases and hormonal changes can contribute to the onset of osteoarthritis. A multifactorial condition, understanding the factors that cause osteoarthritis is imperative for developing effective prevention and management strategies. Increased awareness of these causes can aid individuals in making informed decisions regarding their joint health and overall lifestyle choices.
Recognizing the Symptoms of Osteoarthritis
Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage, leading to various noticeable symptoms. Understanding these symptoms can greatly assist individuals in recognizing the condition early and seeking appropriate care. One of the primary indicators of osteoarthritis is joint pain, which typically worsens with activity and improves with rest. This pain can be localized in particular joints, such as the knees, hips, hands, and spine.
In addition to pain, stiffness is another common symptom of osteoarthritis. Individuals may experience stiffness, particularly after periods of inactivity such as sitting for extended times or upon waking in the morning. This stiffness usually diminishes with gentle movement but may reoccur after prolonged periods of inactivity. Swelling around the affected joints is also a typical manifestation of this condition. This swelling can result from inflammation and an increase in joint fluid that often accompanies cartilage degeneration.
Reduced flexibility is another critical sign, where affected individuals may find it difficult to move their joints through their full range of motion. This limitation in flexibility can lead to difficulty in performing daily activities such as walking, climbing stairs, or even gripping objects. Symptoms of osteoarthritis often fluctuate in severity; individuals may experience periods of exacerbation followed by those of relative relief. Recognizing when these symptoms become more persistent or severe is vital. Signs indicating a need for medical intervention include increased pain intensity that disrupts daily life, noticeable joint deformity, or signs of systemic issues such as fever and fatigue.
Commonly asked questions regarding symptom management include inquiries about the effectiveness of over-the-counter pain relievers or the benefits of physical therapy and low-impact exercises, which are often recommended to alleviate discomfort. Understanding and managing these symptoms can be crucial in maintaining one’s quality of life while living with osteoarthritis.
Risk Factors for Developing Osteoarthritis
Osteoarthritis, a degenerative joint disease, is influenced by multiple risk factors that vary among individuals. Age is one of the most significant risk factors, as the likelihood of developing osteoarthritis increases with advancing years. The wear and tear experienced by joints over time contributes to the degeneration of cartilage, leading to pain and stiffness. Typically, individuals over the age of 50 are at a higher risk, although earlier onset can occur, especially when other risk factors are present.
Gender also plays a crucial role in susceptibility to osteoarthritis. Research indicates that women are more likely to develop this condition, particularly after menopause. Hormonal changes may contribute to the increased risk, affecting joint health. Furthermore, individuals with a family history of osteoarthritis may have a genetic predisposition, making them more susceptible to developing the disease. Understanding one’s ancestry can provide insights into the likelihood of osteoarthritis, guiding preventive measures.
Obesity is another critical risk factor for osteoarthritis. Excess body weight adds additional stress to weight-bearing joints, such as the hips and knees. This increased pressure accelerates the breakdown of cartilage, heightening the potential for osteoarthritis. Moreover, lifestyle choices significantly influence the development of this condition. Inadequate physical activity can weaken muscles surrounding the joints, while repetitive joint stress from certain occupations may also increase the risk. Engaging in regular exercise can help maintain joint function and potentially alleviate some of the pressures faced.
Prior joint injuries are also noteworthy risk factors, as they can result in altered joint mechanics and increase the chances of cartilage breakdown. Understanding these contributing factors is essential for prevention and management. For those concerned about their risk levels, consulting an orthopedic doctor for arthritis near me can provide tailored advice and treatment options.
Treatment Options for Osteoarthritis: Non-Surgical and Surgical Approaches
Management of osteoarthritis (OA) encompasses a blend of non-surgical and surgical approaches tailored to the individual needs of patients. Non-surgical treatments serve as the first line of defense in alleviating symptoms and enhancing the overall quality of life. One widely utilized method is physical therapy, which focuses on improving mobility, increasing strength, and reducing stiffness through tailored exercise regimens. Physical therapists may introduce specific exercises designed to minimize the strain on afflicted joints while promoting joint function.
Lifestyle modifications also play a significant role in managing OA symptoms. Weight loss, for instance, can significantly reduce pressure on weight-bearing joints like the knees and hips. Dietary changes may enhance overall joint health, particularly with the inclusion of omega-3 fatty acids known for their anti-inflammatory properties. Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids can also provide substantial relief from pain and inflammation associated with osteoarthritis. Patients are often encouraged to discuss medication plans with their healthcare providers to navigate potential side effects effectively.
In certain situations where non-surgical methods yield insufficient relief, surgical interventions may be necessary. Joint replacement surgery is a notable surgical option for patients experiencing severe degenerative changes, significantly impacting their mobility. This procedure substitutes the damaged joint with artificial components, thereby alleviating pain and enhancing function. Another option, arthroscopy, involves the insertion of a small camera into the joint for diagnosis and treatment of cartilage damage or loose fragments. Each surgical approach aims to restore function and reduce pain, emphasizing the necessity of an individual-centered treatment plan.
Understanding the spectrum of treatment options is essential for empowering individuals with osteoarthritis. Engaging in discussions with healthcare professionals, exploring best treatments for osteoarthritis pain, and considering both non-surgical and surgical approaches can assist patients in making informed decisions tailored to their circumstances.
Frequently Asked Questions?
Q. What is osteoarthritis?
Ans. Osteoarthritis (OA) is a degenerative joint disease that occurs when the protective cartilage cushioning the ends of bones wears down over time, leading to pain, stiffness, and reduced mobility.
Q. What causes osteoarthritis?
Ans. Osteoarthritis is primarily caused by wear and tear of the joints over time. Factors like aging, joint injuries, repetitive stress, and genetic predisposition contribute to cartilage breakdown.
Q. What are the common symptoms of osteoarthritis?
Ans. The most common symptoms include joint pain, stiffness (especially after rest), swelling, reduced range of motion, and a grinding sensation (crepitus) in the affected joints.
Q. Which joints are most commonly affected by osteoarthritis?
Ans. Osteoarthritis most commonly affects the knees, hips, hands, and spine. However, it can develop in any joint that experiences repetitive stress or previous injury.
Q. What are the risk factors for osteoarthritis?
Ans. Risk factors include aging, obesity, joint injuries, genetics, repetitive joint stress (due to occupation or sports), gender (women are at higher risk), and bone deformities.
Q. How is osteoarthritis diagnosed?
Ans. Doctors diagnose osteoarthritis based on symptoms, physical examination, imaging tests (X-rays, MRI), and sometimes joint fluid analysis to rule out other conditions.
Q. Can osteoarthritis be cured?
Ans. There is no cure for osteoarthritis, but treatments can help manage symptoms and slow disease progression. Lifestyle changes, medications, physical therapy, and in severe cases, surgery can provide relief.
Q. What are the non-surgical treatment options for osteoarthritis?
Ans. Non-surgical treatments include pain relievers (NSAIDs, acetaminophen), physical therapy, weight management, exercise, joint injections (corticosteroids, hyaluronic acid), and lifestyle modifications.
Q. When is surgery recommended for osteoarthritis?
Ans. Surgery is considered when non-surgical treatments fail to relieve pain and improve mobility. Common surgical options include joint replacement (hip/knee), arthroscopy, or osteotomy (realigning bones).
Q. How can osteoarthritis be prevented or managed effectively?
Ans. Preventive measures include maintaining a healthy weight, engaging in regular low-impact exercises, avoiding joint overuse, using proper body mechanics, and following a balanced diet rich in anti-inflammatory foods.