What is Guillain-Barré Syndrome?
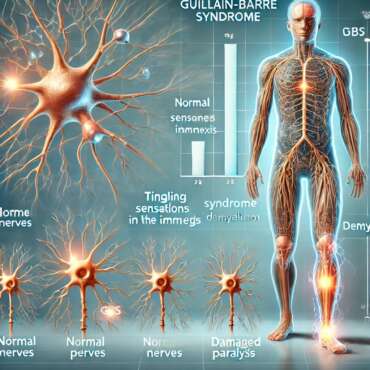
Guillain-Barré Syndrome (GBS) is a rare and potentially disabling autoimmune disorder that primarily affects the peripheral nervous system. Characterized by the body’s immune system mistakenly attacking its own nerve cells, GBS often results in muscle weakness and can lead to paralysis in severe cases. The onset of symptoms can be rapid, typically escalating within days to weeks following an infection, often respiratory or gastrointestinal in nature. This makes early recognition and treatment critical.
Common symptoms of GBS include tingling sensations, weakness that starts in the legs and ascends to upper body, and decreased reflexes. Some patients may experience pain or changes in sensation. In more severe instances, muscle weakness can progress to the point where patients require assistance with daily activities or may even necessitate mechanical ventilation if respiratory muscles are affected. The progression of GBS varies significantly among individuals, with some recovering completely within weeks or months, while others may have lasting effects and require extensive rehabilitation.
GBS can affect individuals of all age groups, but it predominantly occurs in adults, with a slight preference for males. The condition can arise after certain infections, vaccination, or for seemingly no apparent reason at all. Though these triggers are associated with the syndrome, the precise cause of GBS remains largely unknown. It is important to distinguish Guillain-Barré Syndrome from other neurological conditions, such as multiple sclerosis or myasthenia gravis, as GBS primarily involves acute inflammatory demyelination of the peripheral nerves. Comprehensive medical evaluation is essential for a correct diagnosis and appropriate management of the condition.
How Guillain-Barré Syndrome Affects the Body
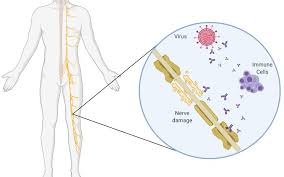
Guillain-Barré Syndrome (GBS) primarily affects the peripheral nervous system, where the immune system inadvertently attacks the very nerves that transmit signals from the brain to various parts of the body. This autoimmune condition begins with an infectious trigger, which can warrant the immune response to mistakenly target nerve cells, particularly the myelin sheath that covers them. The degeneration of this protective layer leads to disrupted communication between the nervous system and muscles, resulting in muscle weakness and sensory impairments.
The most characteristic feature of GBS is its variable onset. It can manifest as mild weakness in the limbs, which may progress to more severe symptoms, including paralysis. Initial symptoms often involve a tingling sensation in the extremities, followed by a symmetrical weakness that may ascend, affecting the legs before progressing to the arms and trunk. As the condition evolves, patients may experience difficulty in walking, and in advanced cases, may require assistance with basic functions. The severity of symptoms can fluctuate significantly from one individual to another, with some experiencing full recovery while others are left with long-term disabilities.
Understanding the implications of GBS is crucial for both patients and caregivers. The syndrome can quickly escalate into life-threatening conditions when the weakness affects the respiratory muscles, necessitating immediate medical intervention. Furthermore, the unpredictable nature of the illness can lead to psychological stress for both the affected individuals and their families. As such, recognizing the early signs and symptoms and seeking prompt treatment can be pivotal. This awareness enables better preparedness for the potential challenges associated with GBS, providing a degree of reassurance for patients navigating this complex condition.
Causes of Guillain-Barré Syndrome
Guillain-Barré Syndrome (GBS) is primarily precipitated by infections, with a significant number of cases following respiratory or gastrointestinal illnesses. Of particular note are infections caused by the Campylobacter jejuni bacterium, which is often associated with food poisoning. Other viral infections have also been linked to the onset of GBS, including the influenza virus and more recently, the Zika virus. These pathogens may trigger an autoimmune response where the body’s immune system mistakenly attacks peripheral nerves, leading to the characteristic muscle weakness seen in GBS patients.
In addition to infections, certain vaccinations have been investigated for their potential role in triggering GBS. For example, studies conducted after the 1976 swine flu vaccination campaign raised concerns about an association between the vaccine and an increased risk of developing GBS. While this association remains contentious, it is important to note that vaccines are generally safe and the incidence of GBS after vaccination is extremely low, outweighing the benefits of immunization against serious illnesses.
Environmental factors are also being studied for their contribution to the risk of developing GBS. Exposures to certain chemicals or substances may play a role in some individuals, although specific links are still being evaluated. On the genetic front, emerging research suggests that hereditary factors may predispose some individuals to GBS. Genetic markers could help identify those at higher risk, thus allowing for better monitoring and early intervention strategies.
Ultimately, while the exact causes of Guillain-Barré Syndrome remain complex and not fully understood, ongoing research continues to explore the interplay between infections, environmental influences, and genetic susceptibility in the development of this debilitating condition.
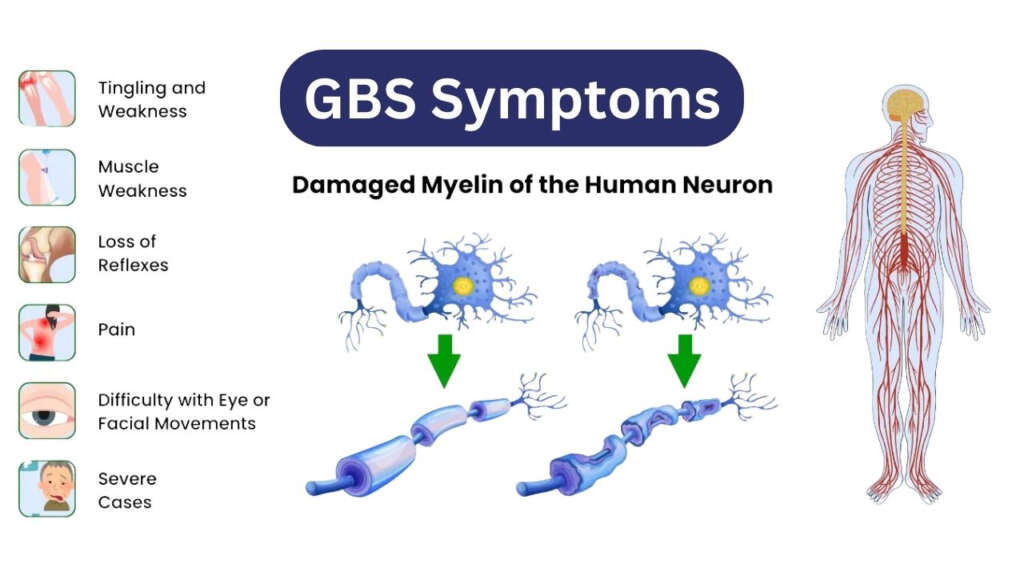
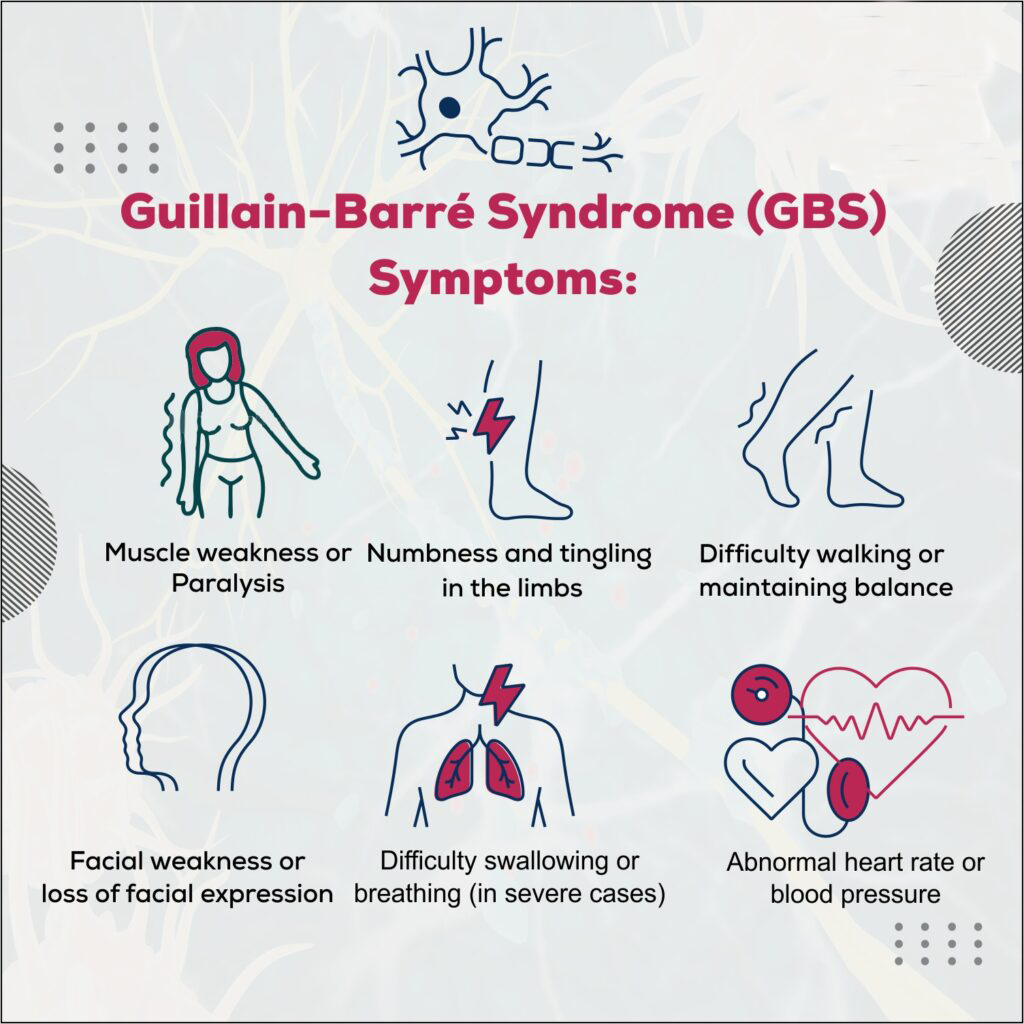
Identifying the Symptoms of Guillain-Barré Syndrome
Guillain-Barré Syndrome (GBS) is an autoimmune disorder that primarily affects the peripheral nervous system, leading to a range of symptoms which can vary in severity and progression. Early identification of these symptoms is crucial for timely medical intervention. Initial signs often include tingling sensations, commonly referred to as paresthesia, which may start in the fingers and toes, gradually spreading to other parts of the body. This sensation can feel like pins and needles and may be mistaken for less serious conditions.
Alongside tingling, muscle weakness is a predominant symptom of GBS. Individuals might experience diminishing strength in one or both legs, which can result in difficulty walking or climbing stairs. In more advanced stages, this weakness can extend to the upper body and even affect respiratory muscles, leading to life-threatening complications. Typically, muscle weakness progresses in a symmetrical pattern, meaning both sides of the body are affected simultaneously. Such a progression is often observed over days to weeks.
Another critical sign is the loss of reflexes, which may become noticeable during a physical exam. Many patients and their families report that reflexes seem diminished or absent entirely. In some cases, muscle pain and tenderness can accompany these symptoms, adding to the discomfort experienced by the patient. The overall onset of symptoms can vary significantly; while some individuals may develop symptoms rapidly over a few hours, others may notice a gradual development occurring over weeks.
Given the potentially serious nature of GBS, recognizing these early indicators is vital. Individuals experiencing unexplained muscle weakness or sensory changes should seek medical attention promptly. Early diagnosis increases the likelihood of effective treatment and improves overall outcomes for those affected by this syndrome.
Diagnosis of Guillain-Barré Syndrome
Diagnosing Guillain-Barré Syndrome (GBS) is a multi-step process that requires careful clinical evaluation, as the symptoms can often mimic those of other neurological disorders. Initially, healthcare professionals conduct a thorough patient history and physical examination, focusing on the onset and progression of symptoms such as muscle weakness, tingling, or numbness. The clinical evaluation is crucial, as GBS typically presents with a symmetrical ascending weakness starting from the legs and moving upward, which helps differentiate it from other potential conditions.
One of the key diagnostic tests performed is a lumbar puncture. This procedure involves collecting cerebrospinal fluid (CSF) to assess for albuminocytologic dissociation, a characteristic finding in GBS. In this condition, the protein level in the CSF is elevated while the white blood cell count remains normal, which distinguishes GBS from other inflammatory or infectious diseases of the nervous system.
In conjunction with lumbar puncture, nerve conduction studies (NCS) and electromyography (EMG) are essential tools for confirming a GBS diagnosis. NCS evaluates the electrical activity of the nerves and determines the speed of nerve conduction, while EMG assesses muscle response to nerve stimulation. Slowed conduction velocities and specific patterns of muscle response can suggest GBS and help exclude other disorders such as multiple sclerosis or myasthenia gravis.
The importance of timely and accurate diagnosis in GBS cannot be overstated, as early identification significantly improves patient outcomes. Prompt initiation of treatments such as intravenous immunoglobulin (IVIG) or plasmapheresis can hasten recovery and reduce the severity of the disease. Therefore, a systematic approach involving clinical assessment, specialized tests, and collaboration among healthcare providers is critical in diagnosing GBS effectively.
Treatment Options for Guillain-Barré Syndrome
Guillain-Barré Syndrome (GBS) is an acute neurological condition characterized by the rapid onset of muscle weakness and paralysis. The primary objective of treatment is to reduce the severity and duration of the symptoms, ultimately enhancing the chances of recovery. Several treatment options are available, the two most notable being intravenous immunoglobulin (IVIG) and plasmapheresis.
IVIG therapy involves the administration of concentrated doses of immunoglobulin, which can help modulate the immune response that attacks the peripheral nerves in GBS patients. This treatment has been shown to improve symptoms when given within the first two weeks of symptom onset. Common side effects may include headaches, fever, and nausea, but these are typically manageable. It is also essential to monitor patients for possible allergic reactions.
Plasmapheresis, or plasma exchange, is another widely recognized treatment option for GBS. This procedure involves removing the blood plasma that contains the harmful antibodies contributing to nerve damage, followed by replacing it with donor plasma or a plasma substitute. Like IVIG, plasmapheresis is most effective when administered early in the course of the disease. Potential side effects include low blood pressure, infections, and an electrolyte imbalance, necessitating careful monitoring during and after the procedure.
Supportive care plays a vital role in the management of GBS. This includes measures such as physical and occupational therapy, respiratory support if required, and adequate nutrition to support overall health and recovery. A multidisciplinary approach involving neurologists, physiotherapists, dietitians, and occupational therapists is crucial in addressing the diverse needs of patients.
Rehabilitation strategies, including functionally focused exercises and muscle strengthening activities, aim to restore mobility and improve daily functioning following an episode of GBS. Early initiation of rehabilitation can significantly impact the recovery trajectory, emphasizing the importance of a comprehensive management plan tailored to each patient’s needs.
Long-Term Outlook and Recovery from Guillain-Barré Syndrome
Guillain-Barré Syndrome (GBS) presents a variable long-term outlook for those affected. Recovery timelines can differ considerably, with many individuals experiencing significant improvement within weeks to months following onset. However, it is important to note that some patients may continue to face persistent weakness, fatigue, or neuropathic pain for years after the initial episode. Often, recovery can take several months to years, with the majority of individuals seeing significant regains within a year. Yet, a small percentage may endure long-term effects, highlighting the unpredictable nature of this condition.
Several factors influence the recovery process from Guillain-Barré Syndrome. The severity of symptoms at onset, the patient’s age, and any pre-existing health conditions play critical roles in determining the prognosis. Younger individuals typically have a better recovery rate compared to older adults. Additionally, those who experienced more severe initial symptoms may face a prolonged recovery period. Timely medical intervention, including treatments such as intravenous immunoglobulin (IVIG) or plasmapheresis, can also positively impact outcomes and expedite recovery.
The psychological effects of GBS should not be overlooked. Many individuals grapple with emotional distress, anxiety, and depression due to significant physical impairment and lifestyle changes. Recognizing the need for mental health support during recovery is essential, as psychological well-being directly influences physical rehabilitation progress. Ongoing support from healthcare providers, psychologists, and support groups can foster a positive recovery environment, addressing both mental and emotional aspects of living with GBS.
Continued monitoring for potential complications is vital. Regular follow-up appointments with healthcare professionals enable the management of any lingering issues and promote the best possible patient outcomes. Overall, the long-term outlook for individuals with Guillain-Barré Syndrome varies, but many can achieve substantial recovery with proper support and monitoring.
Living with Guillain-Barré Syndrome: Support and Resources
Living with Guillain-Barré Syndrome (GBS) can be an overwhelming experience, both physically and emotionally. It is crucial for patients and their families to have access to a variety of support systems and resources to navigate this challenging journey. Emotional and psychological support plays a significant role in recovery, as coping with the unpredictable nature of GBS can often lead to feelings of isolation and anxiety.
Support groups provide a vital platform for individuals affected by GBS, enabling them to connect with others who share similar experiences. These groups serve as an invaluable resource for exchanging coping strategies and finding encouragement. Organizations such as the GBS/CIDP Foundation International offer access to community resources, online forums, and local support meetings for individuals and families coping with GBS.
In addition to support groups, professional counseling can be beneficial. Mental health professionals can provide tailored strategies to help manage the emotional turmoil that may arise during the ongoing recovery process. Family members of those diagnosed with GBS may also benefit from counseling, as they navigate their own feelings of concern and helplessness while caring for their loved ones.
Furthermore, online resources and educational materials can empower patients and families by providing them with reliable information about GBS. Various health organizations and academic institutions have developed comprehensive guides that outline the symptoms, potential treatments, and coping mechanisms for living with GBS. Engaging with this type of information fosters a greater understanding of the illness, which can alleviate some anxiety surrounding the diagnosis.
Lastly, it’s important to develop a support network that encompasses friends, family, and medical professionals. Regular communication and updates about progress can foster a sense of shared accountability and connection, ultimately enhancing the overall emotional well-being of those affected by Guillain-Barré Syndrome.
Preventing Guillain-Barré Syndrome: Myths and Facts
Guillain-Barré Syndrome (GBS) is a relatively rare but concerning neurological disorder characterized by the body’s immune system attacking peripheral nerves. This condition often raises questions regarding its prevention, especially surrounding commonly held misconceptions. One prevalent myth is that vaccinations, particularly the influenza vaccine, directly cause GBS. Scientific research consistently demonstrates that the risk of developing GBS after vaccination is exceedingly low, substantially outweighed by the benefits of immunization in preventing severe illness. Vaccination remains a key preventive health measure, particularly for those at higher risk of complications.
Another misconception posits that GBS can be easily contracted through infection. While it’s true that certain infections, such as Campylobacter jejuni or Zika virus, can trigger GBS, not everyone who encounters these pathogens will develop the syndrome. Understanding that infections are merely triggers rather than direct causes is essential in mitigating fear associated with GBS. Individuals can maintain their health by practicing effective hygiene and receiving prompt medical attention for infections, thus indirectly reducing the risk of GBS.
Staying informed about risk factors is crucial for prevention. While the exact cause of GBS remains unknown, awareness of conditions that may increase risk can help individuals recognize warning signs early. It is advisable to consult healthcare professionals regarding concerns and to avoid relying solely on anecdotal accounts or unverified sources for medical information. Reliable resources, including health agencies and reputable medical journals, provide updated information regarding GBS and its correlation with infections and vaccinations.
By dispelling myths and emphasizing factual information, individuals can enhance their understanding of Guillain-Barré Syndrome. Promoting awareness and knowledge is vital in reducing stigma and empowering people to make informed health decisions, particularly regarding vaccinations and infection prevention strategies.
Frequently Asked Questions?
Q. What is Guillain-Barré Syndrome (GBS)?
Ans. GBS is a rare neurological disorder in which the body’s immune system mistakenly attacks the peripheral nerves, leading to muscle weakness, numbness, and, in severe cases, paralysis.
Q. What causes Guillain-Barré Syndrome?
Ans. The exact cause is unknown, but GBS is often triggered by infections (such as the flu, COVID-19, or Campylobacter bacteria), surgery, or, in rare cases, vaccinations.
Q. What are the early symptoms of GBS?
Ans. The first symptoms typically include tingling, numbness, and weakness in the legs, which can spread to the upper body. Some patients experience difficulty walking, coordination issues, or loss of reflexes.
Q. How is Guillain-Barré Syndrome diagnosed?
Ans. Doctors diagnose GBS through a combination of medical history, neurological exams, nerve conduction studies, lumbar puncture (spinal tap), and electromyography (EMG) tests.
Q. Is Guillain-Barré Syndrome contagious?
Ans. No, GBS is not contagious. It is an autoimmune reaction rather than an infectious disease.
Q. What are the treatment options for GBS?
Ans. There is no cure, but treatments like intravenous immunoglobulin (IVIG) therapy and plasma exchange (plasmapheresis) can help reduce the severity and speed up recovery. Supportive care, including physical therapy, is also essential.
Q. Can Guillain-Barré Syndrome be fatal?
Ans. While rare, GBS can be life-threatening if it affects breathing muscles. Some patients require ventilator support in severe cases. However, with proper medical care, most people recover.
Q. How long does it take to recover from GBS?
Ans. Recovery time varies. Some people recover within a few months, while others may take years. Around 70-80% of patients regain full mobility, but some may experience long-term weakness or fatigue.
Q. Can Guillain-Barré Syndrome recur?
Ans. Recurrence is rare but possible. Around 3-5% of people with GBS may experience symptoms again later in life.
Q. Can GBS be prevented?
Ans. There is no known way to prevent GBS. However, reducing the risk of infections, staying healthy, and getting timely medical attention if symptoms appear may help.