Understanding Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a chronic inflammatory disorder that primarily affects the joints, but it can also impact other systems within the body, including the skin, lungs, and cardiovascular system. This autoimmune condition arises when the immune system mistakenly attacks the synovium, the lining of the membranes that surround the joints. The resulting inflammation leads to swelling and pain, often causing joint damage over time.
The exact cause of rheumatoid arthritis remains unclear, though genetic factors, environmental influences, and hormonal changes may play roles in its development. Symptoms of RA can vary significantly among individuals but typically include prolonged morning stiffness, joint swelling, and fatigue. Symptoms often manifest symmetrically, affecting both sides of the body, and can lead to significant impairment in daily activities.
Conventional treatment options for rheumatoid arthritis aim to relieve symptoms and reduce inflammation while preventing further joint damage. Nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), and corticosteroids are commonly prescribed to manage inflammation and pain. However, these treatments can come with limitations, including potential side effects and the need for long-term use. Some patients may also experience inadequate relief from conventional medications, leading to a chronic cycle of pain and disability.
Moreover, long-term use of medications like DMARDs can pose risks such as increased susceptibility to infections and organ damage. The challenge in managing rheumatoid arthritis lies in the variability of responses to existing therapies, emphasizing the need for innovative approaches. As patients and healthcare providers alike seek more effective solutions, exploring alternative treatments, such as stem cell therapy, emerges as a promising avenue worth considering.
What is Stem Cell Therapy?
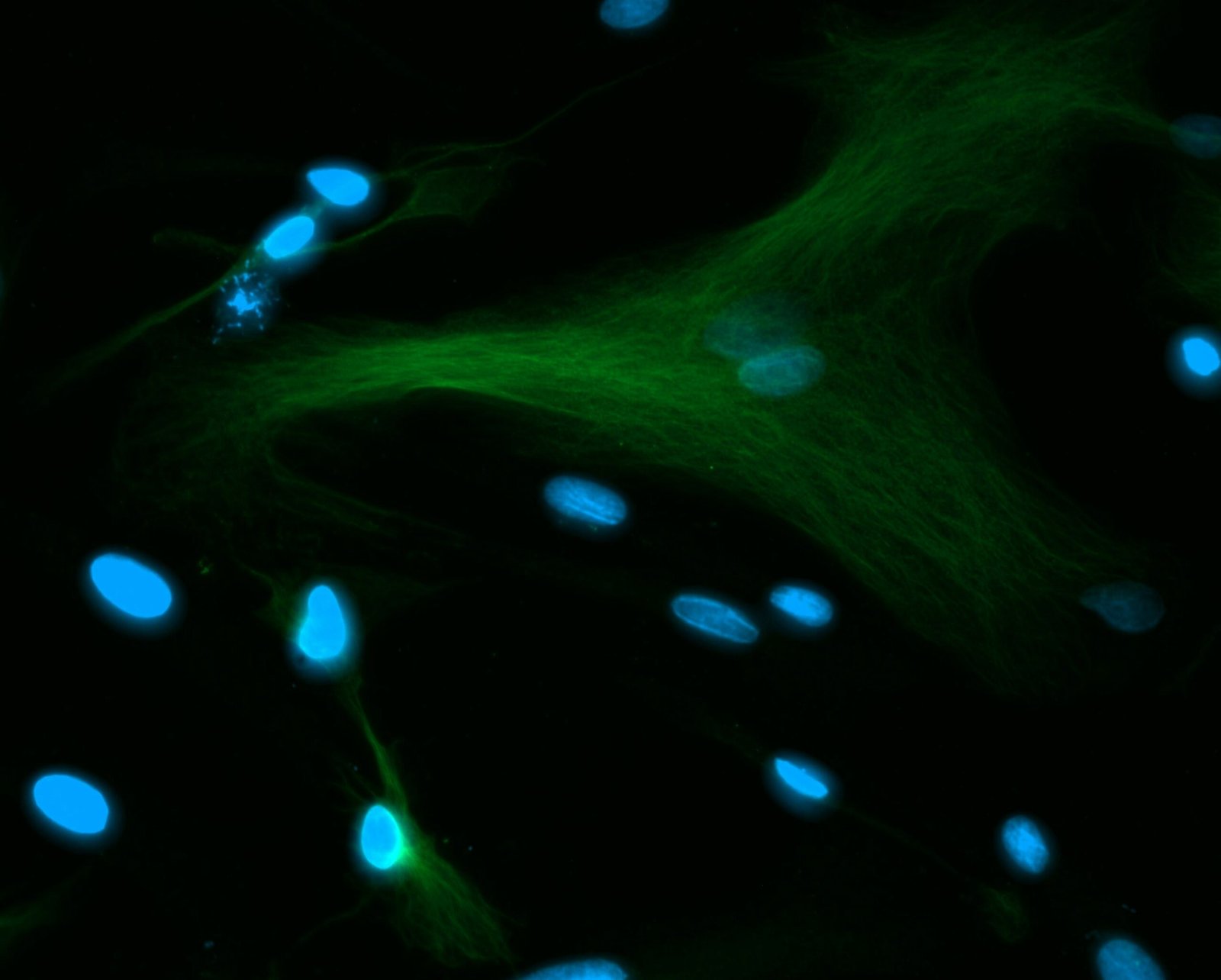
Stem cell therapy represents a groundbreaking approach in regenerative medicine that utilizes the unique properties of stem cells to repair and regenerate damaged tissues. Stem cells are undifferentiated cells with the remarkable ability to differentiate into various cell types, including those essential for repairing damaged tissues in conditions such as rheumatoid arthritis. This therapy leverages the understanding of stem cells’ regenerative potential to treat degenerative diseases, particularly autoimmune disorders characterized by chronic inflammation and tissue destruction.
There are mainly two types of stem cells utilized in therapies: embryonic stem cells and adult stem cells. Embryonic stem cells, derived from early-stage embryos, have the ability to develop into any type of cell in the body. Although they hold significant promise, their use raises ethical and legal concerns. Adult stem cells, on the other hand, are found in various tissues, including bone marrow and adipose (fat) tissue. They are more limited in their differentiation potential compared to embryonic stem cells, but they are pivotal in maintaining tissue homeostasis and have shown great potential in the treatment of arthritis.
The therapeutic process of stem cell therapy for rheumatoid arthritis begins with the extraction of stem cells, which can be harvested from the patient’s own body or from a donor. Once extracted, the cells are processed and concentrated before application. The administration can be done through injections directly into the affected joints or intravenously, allowing the cells to home in on the sites of inflammation and tissue injury. Continuous monitoring of the patient’s response to treatment is crucial, as it helps in evaluating the therapy’s efficacy and making necessary adjustments to improve outcomes.
Current Research and Clinical Evidence
Recent studies and clinical trials have significantly contributed to our understanding of stem cell therapy as a treatment for rheumatoid arthritis (RA). Researchers have explored various types of stem cells, including mesenchymal stem cells (MSCs) and hematopoietic stem cells (HSCs), and their effects on disease progression and symptom relief. A notable trial published in a leading rheumatology journal reported that patients receiving MSC therapy exhibited a substantial reduction in disease activity scores. These improvements were measured against baseline assessments, with many participants experiencing a marked decrease in joint pain and inflammation.
In addition to symptom improvement, studies have also focused on the quality of life of RA patients undergoing stem cell therapy. Findings indicate that individuals treated with stem cells report higher levels of overall well-being and functional capacity. This aligns with data showing that patients receiving traditional treatments, such as methotrexate or biologics, often experience only moderate relief from their symptoms. The comparative success rates suggest that stem cell therapy may provide a more effective alternative for some patients.
However, it is crucial to consider the potential risks and side effects associated with stem cell therapy. Clinical trials have reported complications such as infection, immune reactions, and unintended tissue growth. These risks underline the necessity for thorough patient evaluation and counseling prior to treatment. Additionally, long-term effects of stem cell therapies are still being studied, which is essential for a complete understanding of their safety and effectiveness in managing RA.
In summary, while current research demonstrates promising results for stem cell therapy in treating rheumatoid arthritis, a careful examination of success rates, quality of life improvements, and potential risks is essential for informed decision-making regarding this innovative treatment option.
Future Perspectives and Considerations
As research into stem cell therapy for rheumatoid arthritis (RA) continues to evolve, the future holds significant promise. Ongoing studies are exploring various aspects of this treatment modality, including the efficacy and safety of different stem cell types, including mesenchymal stem cells (MSCs) and hematopoietic stem cells (HSCs). Clinical trials are underway to assess optimal dosages, delivery methods, and patient selection criteria, aimed at identifying which populations may benefit most from stem cell interventions. These advancements signal a hopeful trend toward more effective management of rheumatoid arthritis, potentially improving quality of life for millions worldwide.
Technological innovations also play a crucial role in the development of effective stem cell therapies. Regenerative medicine technologies, such as gene editing and tissue engineering, are being integrated into stem cell therapies to enhance their effectiveness. Moreover, advances in imaging techniques and biomarker identification have the potential to refine patient selection and monitor therapeutic outcomes more accurately, making future treatments more personalized and targeted.
However, the path to wider adoption is not without its challenges. Ethical considerations surrounding stem cell research continue to spark debate, particularly regarding the sources of stem cells. The moral implications of embryonic stem cell use, alongside issues related to consent, necessitate careful deliberation. Furthermore, regulatory hurdles can impede the translation of research into practice. Policymakers are tasked with creating frameworks that both protect patients and promote innovation in stem cell therapies.
For patients considering stem cell therapy as a treatment option for rheumatoid arthritis, it is essential to remain informed. Engaging with healthcare providers, participating in discussions about ongoing clinical trials, and following reputable sources of information can empower patients to make educated decisions. With a combination of scientific advancement and ethical stewardship, stem cell therapy could represent a pivotal shift in the management of RA, fostering hope for improved outcomes in the future.
Frequently Asked Questions?
Q. What is stem cell therapy, and how does it work for rheumatoid arthritis?
Ans. Stem cell therapy involves using stem cells, primarily mesenchymal stem cells, to promote tissue repair and reduce inflammation in joints affected by rheumatoid arthritis. The therapy aims to target the immune response and reduce joint damage by introducing cells that can potentially rebuild damaged tissue.
Q. Can stem cell therapy cure rheumatoid arthritis or just alleviate symptoms?
Ans. Currently, stem cell therapy is not considered a cure for rheumatoid arthritis but may provide symptom relief by reducing inflammation and slowing disease progression. It helps alleviate pain, improves joint function, and enhances quality of life for many patients.
Q. How is stem cell therapy different from traditional treatments for rheumatoid arthritis?
Ans. Traditional treatments, such as NSAIDs, DMARDs, and biologics, primarily manage symptoms and slow disease progression. Stem cell therapy, however, focuses on regenerating damaged tissues and modulating the immune system, offering a more regenerative approach.
Q. What types of stem cells are used in the treatment of rheumatoid arthritis, and where are they sourced from?
Ans. Mesenchymal stem cells (MSCs) are most commonly used for rheumatoid arthritis. They can be derived from various sources, such as the patient’s bone marrow or adipose (fat) tissue, as well as donated umbilical cord tissue.
Q. Is stem cell therapy for rheumatoid arthritis safe, and are there any risks or side effects?
Ans. Stem cell therapy is generally considered safe, but risks may include infection, inflammation, or an adverse reaction to the stem cells. Because the treatment is still experimental, long-term risks are not fully known.
Q. What is the procedure for stem cell therapy for rheumatoid arthritis, and how long does it take?
Ans. The procedure usually involves extracting stem cells from the patient (if autologous) or preparing donated cells. The cells are then injected into the affected joints. The whole process typically takes a few hours, and patients may return home the same day.
Q. How long do the effects of stem cell therapy last, and will I need multiple treatments?
Ans. The effects of stem cell therapy vary among individuals, with some experiencing relief for several months to a few years. Repeat treatments may be necessary, depending on symptom recurrence and disease progression.
Q. Are there specific factors or conditions that make someone a good candidate for stem cell therapy in rheumatoid arthritis?
Ans. Ideal candidates are those with moderate rheumatoid arthritis who haven’t fully responded to traditional therapies. Age, general health, and absence of severe joint damage can also influence suitability for stem cell therapy.
Q. What is the success rate of stem cell therapy for rheumatoid arthritis, and how soon can I expect to see results?
Ans. Success rates vary, with some studies showing positive results in reducing pain and inflammation in up to 70% of patients. Improvements may be noticeable within a few weeks, but the full effects can take several months.