What is Fibromyalgia?
Fibromyalgia is a chronic pain condition characterized by widespread musculoskeletal pain, fatigue, sleep disturbances, and cognitive difficulties. This condition affects the way the brain processes pain signals, leading to an amplified sensation of pain across various regions of the body. The hallmark symptom of fibromyalgia is widespread pain, which is often described as an aching or burning sensation that affects multiple areas, including muscles, ligaments, and tendons.
The significance of fibromyalgia lies not only in its painful manifestations but also in its impact on daily life. Individuals affected by fibromyalgia often experience a variety of symptoms beyond pain, including stiffness, fatigue, headaches, and mood disorders such as anxiety or depression. These symptoms can further complicate the overall health and well-being of an individual, making it a challenging condition to manage.
Fibromyalgia is classified as a rheumatic disease, which encompasses conditions that primarily affect the joints, muscles, and soft tissues. Unlike traditional rheumatic diseases that involve inflammation, fibromyalgia does not entail joint damage or recognize specific inflammatory markers. This lack of identifiable physical abnormalities may lead to difficulty in diagnosing the condition, as many healthcare professionals may overlook it due to the absence of clear physical signs.
The prevalence of fibromyalgia varies across different populations. It is estimated that approximately 2–8% of the general population is affected by this chronic pain condition, with a higher incidence found among women compared to men. The condition often leads to significant societal and economic burdens, resulting in increased healthcare costs and loss of productivity. Understanding fibromyalgia and its implications is crucial to providing effective support and management strategies for those who suffer from it.
Common Symptoms of Fibromyalgia
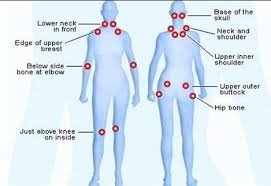
Fibromyalgia is primarily characterized by widespread pain, which is often described as a constant dull ache that lasts for months or years. This hallmark symptom can be exacerbated by stress, weather changes, or physical activity, significantly impacting an individual’s daily life. The pain typically affects both sides of the body and can occur in various locations, such as the shoulders, back, hips, and neck. Individuals often report that the pain can vary in intensity and is sometimes accompanied by tenderness at specific pressure points.
In addition to widespread pain, fatigue is a prevalent symptom of fibromyalgia. Many individuals experience a persistent exhaustion that seemingly cannot be alleviated by rest or sleep. This overwhelming tiredness can hinder participation in everyday activities and may contribute to feelings of frustration and helplessness. The fatigue often intertwines with disrupted sleep patterns. Many individuals suffering from fibromyalgia report difficulties in achieving restorative sleep, which is crucial for overall well-being. Sleep disturbances may include insomnia, frequent awakenings during the night, and restless leg syndrome, further impacting energy levels and mood.
Cognitive difficulties present yet another challenge for those with fibromyalgia. Individuals may experience trouble concentrating, memory problems, and mental clarity issues, which can severely affect work performance and social interactions. Mood disorders are also frequently reported, with many individuals experiencing anxiety and depression as a consequence of living with chronic pain and fatigue. These emotional challenges may exacerbate the perception of physical symptoms, complicating the overall management of the condition. Understanding these diverse symptoms is crucial for both individuals and healthcare providers in adequately addressing and treating fibromyalgia.
Causes of Fibromyalgia: What We Know So Far
Fibromyalgia is a complex chronic pain disorder characterized by widespread musculoskeletal pain and a variety of other symptoms. Understanding the causes of fibromyalgia is crucial for effective management and treatment, yet the origins of this condition remain largely elusive. Research indicates that a combination of genetic predisposition, environmental factors, and psychological elements may contribute to its onset.
Genetic factors seem to play a significant role in fibromyalgia, as studies have shown that the condition often runs in families. Individuals with a family history of fibromyalgia or other chronic pain disorders may be at a higher risk due to inherited traits affecting pain perception or neurological function. This genetic predisposition can interact with environmental triggers, leading to the development of symptoms.
Central sensitization is one theory that has gained prominence in explaining the condition. This phenomenon occurs when the nervous system develops an enhanced response to pain signals. Essentially, the brain may interpret normal sensory input as heightened pain due to an alteration in how pain is processed. This alteration can be influenced by previous trauma, whether physical or emotional, which has been shown to correlate with the development of fibromyalgia.
Moreover, infections and stress are significant risk factors. Certain viral or bacterial infections have been linked to the onset of fibromyalgia symptoms, suggesting that an infectious trigger could activate the disorder in susceptible individuals. Additionally, long-term stress has proven to exacerbate the condition, highlighting the importance of psychological well-being in managing fibromyalgia.
In conclusion, while the exact causes of fibromyalgia are not fully understood, it is evident that a multifaceted interplay of genetic, environmental, and psychological factors contributes to this complex condition. Understanding these various influences can aid in recognizing the symptoms early and seeking appropriate treatment.
Risk Factors for Developing Fibromyalgia
Fibromyalgia is a complex condition influenced by a myriad of risk factors that can make certain individuals more susceptible to its onset. One notable demographic factor is age; research indicates that fibromyalgia is most commonly diagnosed in middle-aged individuals, typically between the ages of 30 and 60. However, it is essential to note that while this age group is at a heightened risk, fibromyalgia can also manifest in younger and older populations.
Gender is another significant factor, as studies consistently show that fibromyalgia is more prevalent in women than in men. The reasons for this disparity are not entirely understood, but hormonal differences may play a role, as well as social and psychological factors that differ between genders. Furthermore, a family history of fibromyalgia can also increase one’s chances of developing the condition. Genetic predispositions may exist, indicating that fibromyalgia can run in families, which suggests a potential hereditary component to the disease.
In addition to demographics, various medical conditions can heighten the risk of developing fibromyalgia. Conditions such as rheumatoid arthritis, lupus, and osteoarthritis have been associated with an increased likelihood of fibromyalgia symptoms. Individuals suffering from these chronic illnesses may find that the risks amplify due to shared pathophysiological mechanisms, such as inflammation and pain sensitivity.
Lifestyle factors also play a crucial role in determining the risk of fibromyalgia. Experiences of chronic stress, emotional trauma, or physical injuries can act as triggers for the onset of fibromyalgia. It is well-documented that stress management and emotional well-being are vital in mitigating these risks. Understanding the interplay of these various factors can be critical in not only recognizing but also addressing the potential development of fibromyalgia.