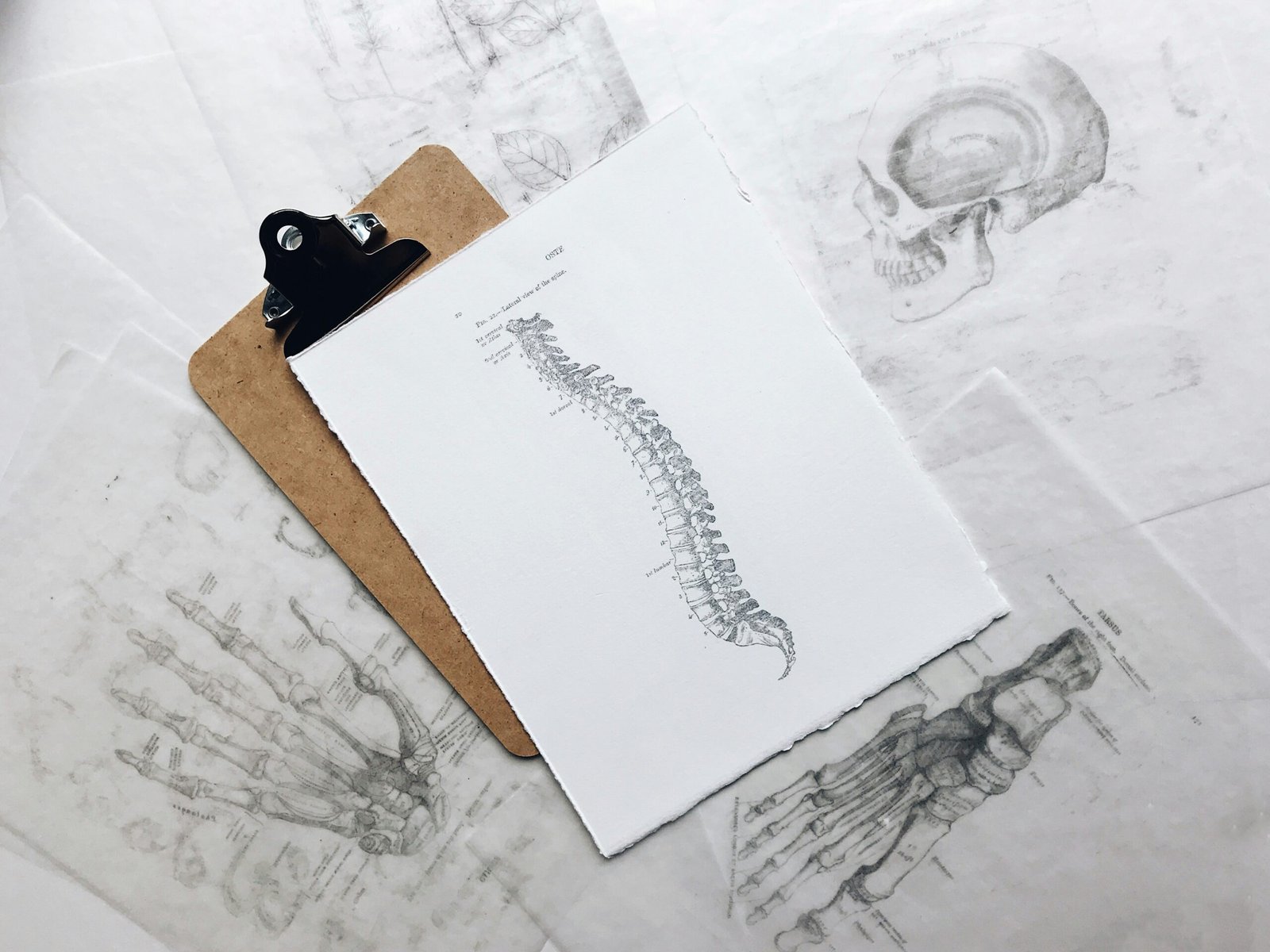
Understanding Spine Surgery: Types and Reasons
Spine surgery encompasses a range of surgical procedures designed to address various spinal conditions. Common types of spine surgery include discectomy, spinal fusion, and laminectomy. Each procedure targets specific spinal issues, offering potential relief from debilitating symptoms and improving overall quality of life.
Discectomy is performed to remove herniated disc material that presses on spinal nerves, often resulting in pain, numbness, or weakness in the limbs. This surgery can effectively relieve nerve compression caused by intervertebral disc herniation, especially in conditions such as a herniated disc or sciatica. By alleviating pressure on the affected nerve, patients frequently experience a significant reduction in pain and an increase in mobility.
Laminectomy, on the other hand, entails the removal of the lamina, the bony arch that forms the back of the vertebra. This procedure is often indicated for patients suffering from spinal stenosis, a condition characterized by narrowed spinal canals that compress the spinal cord and nerves. By removing the lamina, laminectomy helps relieve pressure, thus alleviating symptoms of nerve pain, weakness, and numbness.
Spinal fusion, another prevalent procedure, involves the joining of two or more vertebrae to enhance stability in the spine. This surgery is particularly beneficial for conditions like degenerative disc disease, spondylolisthesis, and spinal deformities. The fusion creates a single, solid bone structure, thereby preventing painful movement between the vertebrae. While it does limit flexibility in the individual segments of the spine, it can significantly improve pain levels and enhance the functionality of the spine in the long term.
Overall, understanding the different types of spine surgeries and the conditions they address is crucial in making informed medical decisions. Each surgical intervention has unique benefits tailored to specific spinal issues, guiding patients toward effective relief from their symptoms.
Identifying Symptoms That May Indicate the Need for Surgery
Determining whether spine surgery is necessary often begins with recognizing specific symptoms that may indicate underlying issues. Chronic pain is one of the most common signs, especially if it persists despite various conservative treatments, such as physical therapy, medication, or injections. This pain may be localized to the back or radiate to other parts of the body, significantly impairing daily activities and overall quality of life.
Another critical factor to consider is the significant loss of mobility. Individuals might experience difficulty in performing routine tasks such as bending, lifting, or even walking. When the spine’s range of motion is compromised, it becomes essential to evaluate if surgical options could restore function and alleviate discomfort.
Neurological symptoms may also serve as red flags for potential spinal conditions. Patients may report tingling, numbness, or weakness in the limbs, which can suggest nerve compression or other serious concerns. These symptoms can indicate conditions like herniated discs or spinal stenosis, necessitating a thorough medical examination to assess the need for surgical intervention.
The severity and duration of these symptoms play a crucial role in decision-making. It is vital for individuals experiencing any of these warning signs to consult a healthcare professional. A comprehensive evaluation will ensure appropriate treatment options are explored, potentially preventing further complications and enhancing the patient’s well-being.
Evaluating Treatment Options: When Surgery Is the Best Choice
Choosing the appropriate treatment for spine issues can be a complex decision, often involving a careful evaluation of both conservative and surgical options. In many cases, healthcare providers will first recommend conservative treatment modalities such as physical therapy, medication, or injections. These approaches aim to alleviate pain and improve function without the need for invasive procedures. However, when conservative measures fail to yield satisfactory improvements or when symptoms worsen, the possibility of spine surgery may need to be explored.
Several critical factors influence the decision to proceed with surgical intervention. First, the severity and type of spinal condition play a significant role. For instance, conditions such as herniated discs, spinal stenosis, or significant spinal instability may warrant surgical correction, especially if they result in debilitating pain or neurological deficits. Additionally, the duration and intensity of symptoms also contribute to the urgency of considering surgery. Patients who have repeatedly experienced severe symptoms over an extended period may find that their quality of life is significantly impacted, prompting the need for surgical options.
Another crucial aspect of the evaluation process is the role of a thorough assessment by a qualified specialist. A comprehensive examination, including imaging studies such as MRIs or CT scans, can provide insight into the underlying cause of the spinal issues. Interdisciplinary consultations may also be valuable; discussing the case with multiple healthcare professionals, such as physical therapists and pain management specialists, can foster a more informed decision-making process. This collaborative approach will ensure that all potential treatment options are thoroughly explored, helping patients understand the risks and benefits associated with each choice.
Ultimately, the decision to undergo spine surgery should be based on a combination of clinical evidence, patient preferences, and a careful evaluation of all treatment alternatives. This multifaceted approach allows for a well-informed decision regarding the best course of action for an individual’s unique circumstances.
What to Expect Before, During, and After Spine Surgery
Preparing for spine surgery involves several crucial pre-operative assessments to ensure the patient’s overall health and readiness for the procedure. Before surgery, patients often undergo a thorough evaluation, which may include imaging studies like MRIs or CT scans, blood tests, and a comprehensive physical examination. These assessments allow the surgical team to gather vital information about the patient’s condition, enabling them to develop a tailored surgical plan. Additionally, patients may be advised to stop certain medications or adjust their diets in the lead-up to the surgery to minimize risks.
During the surgical procedure itself, the approach can vary significantly depending on the specific type of spine surgery being performed. Generally, surgeries may involve techniques such as discectomy, laminectomy, or spinal fusion. Anesthesia will be administered to ensure the patient remains comfortable and pain-free throughout the operation. The duration of surgery varies, but it generally takes a few hours. Surgeons will typically provide patients and their families with updates during the procedure, alleviating some preoperative anxiety.
Post-operative recovery is a vital phase that can significantly influence the overall outcome of spine surgery. Patients may experience pain and discomfort as they begin to heal, and pain management strategies will be implemented to address these challenges. Physical therapy is often recommended to facilitate rehabilitation and improve mobility. The recovery timeline can differ widely based on the complexity of the surgery, with some patients requiring weeks to months for full recovery. Regular follow-up appointments will help monitor progress and address any concerns. Adequate preparation and understanding of the surgical journey can equip patients with the knowledge they need to navigate this important chapter in their healthcare journey.
Frequently Asked Questions?
1. What are the main signs that indicate I might need spine surgery?
Answer: Surgery may be necessary if you experience severe, persistent back or neck pain that doesn’t improve with non-surgical treatments, progressive weakness or numbness in the legs or arms, or difficulty walking or maintaining balance. Spine surgery may also be advised if there’s evidence of nerve compression or structural issues, like herniated discs or spinal stenosis.
2. How can I know if my back pain requires surgery or if non-surgical options are better?
Answer: Non-surgical treatments such as physical therapy, medications, injections, and lifestyle changes are typically tried first. Surgery is usually recommended only when these methods don’t provide relief, or when there is a specific condition, like spinal instability or nerve damage, that requires surgical intervention.
3. What are the most common types of spine surgeries, and how do they differ?
Answer: Common types include discectomy (removing part of a herniated disc), laminectomy (removing part of the bone to relieve nerve pressure), spinal fusion (joining two vertebrae to stabilize the spine), and artificial disc replacement (replacing a damaged disc with an artificial one). Each surgery has a specific goal depending on the condition and symptoms.
4. Are there minimally invasive options for spine surgery?
Answer: Yes, many spine surgeries can now be done with minimally invasive techniques, which use smaller incisions and specialized tools. These options often lead to faster recovery, less pain, and fewer complications, though not all spine conditions are suitable for minimally invasive procedures.
5. What are the risks and benefits of undergoing spine surgery?
Answer: The benefits include relief from chronic pain, improved mobility, and restoration of function. However, risks include infection, bleeding, nerve damage, blood clots, and, in some cases, continued or worsened symptoms. The risk-benefit ratio depends on individual health, the type of surgery, and the surgeon’s expertise.
6. How long is the recovery period after spine surgery, and what can I expect?
Answer: Recovery varies by procedure. Minimally invasive surgeries may have shorter recovery times (a few weeks), while complex procedures like spinal fusion can take months. During recovery, you’ll likely undergo physical therapy, avoid heavy lifting, and gradually increase activity to strengthen the spine and surrounding muscles.
7. Is spine surgery a permanent solution for chronic back pain?
Answer: Spine surgery can provide significant relief, but it may not completely eliminate chronic pain, especially if there are other contributing factors like arthritis. Maintaining a healthy lifestyle, doing strengthening exercises, and following your doctor’s advice can improve long-term outcomes.
8. Are there any alternative therapies that can delay or eliminate the need for spine surgery?
Answer: Yes, therapies like physical therapy, acupuncture, spinal injections, and lifestyle changes can sometimes delay or avoid surgery. Always consult a specialist to explore these options based on your specific condition and overall health.
9. How do I find a qualified spine surgeon and what questions should I ask before surgery?
Answer: Look for a board-certified spine surgeon with experience in the specific procedure you need. Ask about their success rates, complication rates, recovery expectations, and if they recommend minimally invasive options. You may also ask if a second opinion would be beneficial to ensure the best approach.
10. What lifestyle changes can help improve recovery and outcomes after spine surgery?
Answer: Healthy lifestyle changes can make a big difference. Staying active (within guidelines), maintaining a healthy weight, avoiding smoking, and focusing on posture can support spine health. Regular physical therapy exercises and strengthening core muscles are also essential for a smooth recovery and long-term spine health.