What is a Herniated Disk?
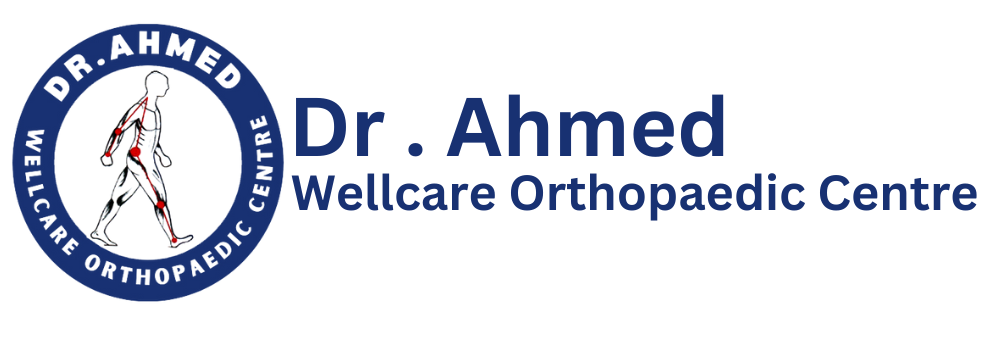
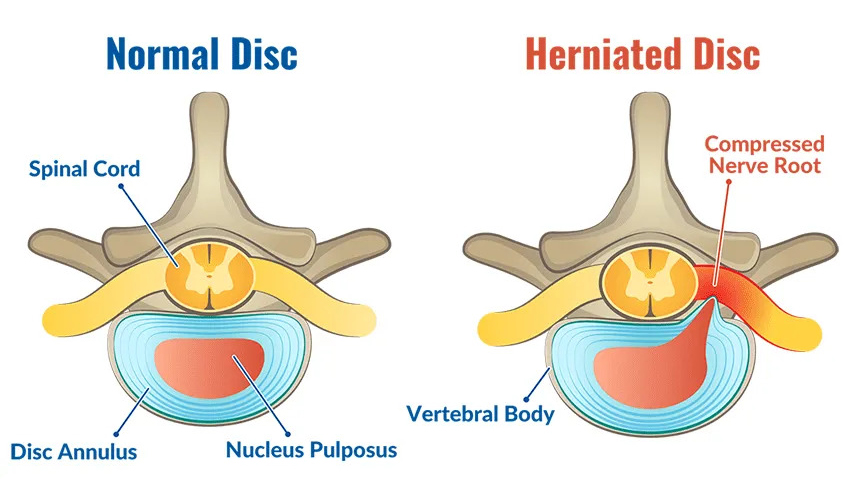
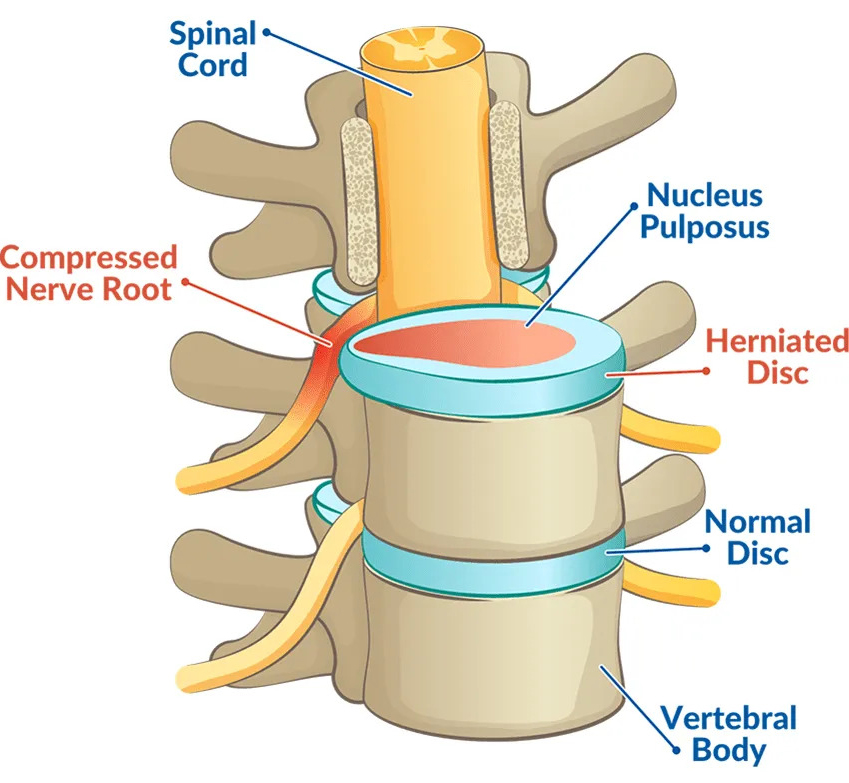
A herniated disk, also referred to as a slipped or ruptured disk, occurs when the inner gel-like core of the intervertebral disk protrudes through a tear in the outer layer. This anatomical structure, composed of the nucleus pulposus and annulus fibrosus, serves as a cushion between the vertebrae in the spine. The primary function of these disks is to absorb shock, providing flexibility and support during movement.
Herniated disks can arise from various factors, one of the most common being spinal degeneration, which typically occurs with age. As individuals grow older, the intervertebral disks lose hydration and elasticity, making them more susceptible to injuries. Other causes may include sudden lifting of heavy objects, strenuous physical activity, or even trauma from accidents, which can result in a herniated disk. Additionally, lifestyle choices such as obesity and sedentary behavior may contribute to the degeneration of spinal structures, leading to the development of herniated disks.
It is essential to note that herniated disks can manifest in different forms. Lumbar herniated disks primarily affect the lower back and often result in pain that radiates to the legs. Conversely, cervical herniated disks occur in the neck region and may cause pain or numbness in the arms and shoulders. Thoracic herniated disks, although less common, affect the upper back and can lead to more serious complications if left untreated. Understanding the underlying mechanisms and types of herniated disks is crucial for proper diagnosis and treatment, highlighting the need for awareness regarding spinal health.
Common Symptoms of a Herniated Disk
A herniated disk, often referred to in medical terms as a slipped or ruptured disk, can manifest a range of symptoms that vary significantly depending on the location of the herniation. The two primary regions where herniated disks occur are the cervical (neck) and lumbar (lower back) areas, with each having distinct symptomatology. In the cervical region, individuals may experience radiating pain that extends into the shoulders and arms. This pain can be accompanied by sensations of numbness or tingling in the fingers, often indicative of nerve involvement. Weakness in the hand or arm is also a common symptom in cases of cervical disk herniation, potentially impacting one’s ability to grip objects.
On the other hand, lumbar herniation primarily affects the lower back and can radiate pain into the buttocks, thighs, and sometimes down the legs, a phenomenon often referred to as sciatica. The intensity of this pain can vary, sometimes described as a sharp or burning sensation, which may worsen with movement. Similar to cervical herniation, numbness or tingling can occur, particularly in the legs or feet, indicating pressure on the associated nerves. Weakness in the leg muscles may also result, making activities such as walking or standing challenging for those affected.
It is essential to note that the symptoms of a herniated disk will greatly depend on the severity of the herniation and the individual’s overall health. Personal experiences vary; some individuals may only experience mild discomfort, while others suffer from debilitating pain and functional limitations. Recognizing these symptoms promptly is crucial for effective treatment and management. By understanding the common signs associated with herniated disks, individuals can seek timely medical intervention, ultimately enhancing their quality of life.
Diagnosing a Herniated Disk
The diagnosis of a herniated disk generally begins with a comprehensive evaluation by a healthcare professional, usually a physician or a specialist in spinal disorders. During the initial consultation, the practitioner will conduct a thorough physical examination, assessing the patient’s medical history, symptoms, and any previous treatments. A detailed account of the pain’s onset, location, intensity, and aggravating or alleviating factors helps in establishing a clear picture of the patient’s condition.
Healthcare professionals may assess the patient’s range of motion and neurological function, which includes testing reflexes, muscle strength, and sensory responses. This examination can reveal signs indicative of nerve compression, which is often associated with a herniated disk. Certain specific tests, such as the straight leg raise test, may also be performed to further evaluate the presence of nerve-related issues affecting the lower back and legs.
While a physical examination can provide valuable insights, imaging tests are crucial to confirm the diagnosis. Magnetic Resonance Imaging (MRI) is widely regarded as the gold standard for visualizing soft tissue structures, including the spinal cord and discs. This imaging technique allows healthcare professionals to observe the size and location of the herniation as well as the potential impact on surrounding nerves. CT scans are another option that can be used, particularly in cases where MRI is unavailable or contraindicated. These scans can help to visualize the bony structures of the spine and identify any contributing factors, such as bone spur formations.
Accurate diagnosis of a herniated disk is essential for creating an effective treatment plan. Misdiagnosis or failure to identify a herniated disk can lead to inappropriate treatments, prolonged pain, and complications. Thus, distinguishing a herniated disk from other spinal issues, such as spinal stenosis or degenerative disc disease, is critical. This requires careful analysis of both the clinical and imaging data, emphasizing the necessity for skilled assessment by a qualified medical professional.
Treatment Options and Management Strategies
When dealing with herniated disks, individuals have access to a variety of treatment options that can help manage symptoms and facilitate recovery. These options can be broadly categorized into conservative methods and more invasive procedures. Initially, conservative treatments are often recommended as the first line of action due to their non-intrusive nature.
Conservative treatments typically include physical therapy, which focuses on strengthening the muscles supporting the spine and improving flexibility and posture. Physical therapists may also employ techniques like ultrasound or electrical stimulation to alleviate pain. Additionally, medications such as non-steroidal anti-inflammatory drugs (NSAIDs) are frequently prescribed to reduce inflammation and manage pain effectively. In some cases, corticosteroid injections may be used to provide temporary relief of severe symptoms.
However, if conservative measures prove ineffective over time, patients may need to consider more invasive options, including surgical interventions. Procedures such as a discectomy, where the herniated portion of the disk is removed, may be warranted for individuals experiencing significant pain or neurological deficits. In more severe cases, spinal fusion might be recommended to provide stability to the spine after the removal of the damaged disk.
In addition to professional medical treatments, self-management strategies can play an essential role in recovery and long-term management of a herniated disk. Education on proper ergonomics, particularly in workplace settings, can help reduce strain on the spine. Furthermore, making lifestyle changes such as maintaining a healthy weight, engaging in appropriate exercises, and regular stretching can significantly contribute to spinal health.
To minimize the risk of future disk herniation, individuals should focus on maintaining proper lifting techniques, avoiding prolonged sitting, and incorporating regular physical activity into their routines. Implementing these preventive measures can aid in promoting overall spinal integrity and well-being.
Frequently Asked Questions?
Q. What Is a Herniated Disk?
Ans. A herniated disk occurs when the soft inner portion of a spinal disk pushes through a tear in its outer layer, irritating nearby nerves and causing pain, numbness, or weakness.
Q. What Causes a Herniated Disk?
Ans. Common causes include:
- Age-related degeneration (disk wear and tear)
- Sudden heavy lifting or twisting movements
- Repetitive strain on the spine
- Traumatic injury
Q. What Are the Symptoms of a Herniated Disk?
Ans. Symptoms depend on the affected location but may include:
- Sharp or radiating pain (back, neck, arms, or legs)
- Numbness or tingling in affected areas
- Muscle weakness
- Pain worsening with movement or prolonged sitting
Q. Where Does a Herniated Disk Commonly Occur?
Ans. Herniated disks most commonly occur in the lower back (lumbar spine) and neck (cervical spine), though they can also affect the mid-back (thoracic spine).
Q. Can a Herniated Disk Heal on Its Own?
Ans. Yes, in many cases, mild to moderate herniated disks improve with time, rest, and conservative treatments. The body can absorb part of the herniation, reducing symptoms naturally over weeks or months.
Q. What Are the Treatment Options for a Herniated Disk?
Ans. Treatment may include:
- Pain management (NSAIDs, corticosteroid injections)
- Physical therapy and targeted exercises
- Heat and ice therapy
- In severe cases, surgery such as microdiscectomy or spinal fusion may be needed
Q. When Should I See a Doctor for a Herniated Disk?
Ans. Seek medical attention if you experience:
- Severe pain that doesn’t improve with rest
- Weakness, numbness, or tingling in the limbs
- Loss of bladder or bowel control (a medical emergency)
Q. Can a Herniated Disk Cause Permanent Nerve Damage?
Ans. In rare cases, if a herniated disk compresses a nerve for too long, it may cause permanent nerve damage, leading to chronic pain, muscle weakness, or mobility issues.
Q. How Can I Prevent a Herniated Disk?
Ans. Prevention tips include:
- Maintaining good posture
- Regular exercise to strengthen core and back muscles
- Lifting heavy objects properly (using legs, not back)
- Avoiding prolonged sitting or repetitive spine strain
Q. Is Surgery Always Necessary for a Herniated Disk?
Ans. No, surgery is usually a last resort if conservative treatments fail after several months, or if there is severe nerve compression causing significant weakness or loss of function.